National Nurses Week Spotlights Most Trusted Profession
Published in nurse.com by Eileen Williamson, MSN, RN
You are celebrated during National Nurses Week for the many contributions you make to the nursing profession and the healthcare of our nation. The word “excellence,” in fact, is one we hear more than any other during Nurses Week.
Hospice Care & Palliative Care – When to use them
Published in parentyourparents.com by Petr Horcik
Hospice a word that is synonymous with “end of life” care. Palliative – a little more confusing and often confused with ‘end of life’. The two are very different therapies but Palliative Care is an offshoot of Hospice.
Hospice is a service for patients who are terminally ill and have decided not to take any more medication that might “cure” them (i.e. chemotherapy for a cancer patient). The focus becomes relief from pain and symptoms and not a cure. There are some who say that going into Hospice means you’re giving up or that you will no longer receive the medical care you need. That is not true – you have chosen to focus on your quality of life not the quantity and the medication used is to do just that.
Study: Hospice Concurrent With Cancer Treatment Reduces Costs
Published in hospicenews.com by Jim Parker
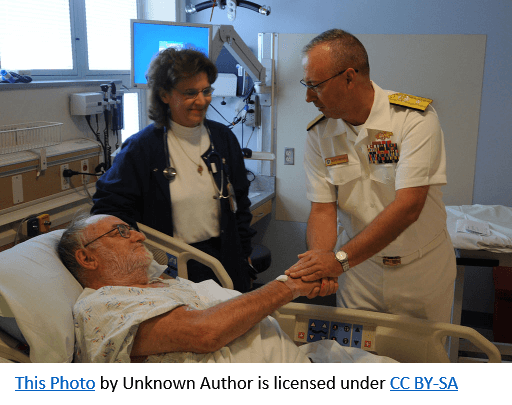
A study of more than 13,000 veterans in Veterans Affairs Medical Centers (VAMCs) found that patients receiving hospice care concurrent with chemotherapy or radiation therapy were less likely to use aggressive treatments or be admitted to intensive care compared to similar patients who were not enrolled in hospice, significantly reducing medical costs.
Unlike organizations reimbursed through the Medicare Hospice Benefit, the Veteran’s Health Administration (VHA) does not require hospice patients to forgo curative care, making VAMCs a prime environment for researching concurrent treatments.
Advanced, palliative care plans important part of life
Published in Cleveland Jewish News by Becky Raspe
It’s best to be prepared in every situation, especially when it’s health-related.
According to Rabbi Akiva Feinstein, director of spiritual care at Montefiore in Beachwood, and Dr. Beth McLaughlin, chief medical officer at Hospice of the Western Reserve in Cleveland, creating a plan for advanced and palliative care makes decisions easier.
What you can expect from hospice care
Published in considerable.com by Walecia Konrad
This service can bring dignity and grace to the end of life

That upset Raiford even more. “You hear the word hospice and you think to yourself, this person is going to die and I don’t want that,” she says. “Worse, you think by agreeing to hospice you’re helping the person die.”
How to Become a Social Worker
Every day, the nation’s 680,000 social workers work to empower and elevate millions of people, including some of the most vulnerable in our society.
National Professional Social Work Month in March 2019 is an opportunity for social workers around the nation and world and their supporters to educate the public about the invaluable contributions of the profession.
Being a social worker is a rewarding profession. Following are tips on how to get into the field and the academic background needed.
Learning Has Shaped Oncology Nurse’s View of Patient Care
Published in oncnursingnews.com by Jean Sellers, MSN, RN
There is an old proverb I’ve heard many times, attributed to several sources: “When the student is ready, the teacher will appear.” Although I was anything but ready to face the concepts of death and dying, in 1990, my teacher appeared. He was 59 years old and presented to the emergency department with sudden onset nausea and vomiting, along with a severe headache. I vividly remember standing outside the thin curtain separating his stretcher from where I stood, dumbfounded, as the doctor introduced the words “temporal mass” and “cerebral edema” into my life.
I wasn’t a nurse then. I was a mother to 2 young girls, and I was not prepared to take care of the man behind the curtain. He was the greatest man I had ever known, the same man whom I would forever refer to as my first patient. My father. His diagnosis was an aggressive glioblastoma, and he lived 9 months from that day. I was forced into a crash course on surgery, radiation therapy, and end-of-life care. His final 2 months were spent in my home. The man who defined a “good day” as 18 holes on a golf course was now confined to a hospital bed in my guest bedroom, wearing diapers.
My family came together with the best of intentions, but we never quite had the conversations we needed to have. Some family members refused to acknowledge he was dying, and others viewed hospice care as giving up. Some did not want to treat his pain with narcotics for fear he would become addicted. I was desperate to find anyone who could help me ensure that my father would not suffer, which finally led me to call the hospice answering service—and brought another teacher in to my life.
The hospice nurse returned my call later that evening. Nothing could have prepared me for the way it felt to feel so completely heard and understood in the midst of that terrifying time. She listened to my concerns, fears, and confusion. She became my lifeline and helped my family to have the difficult conversations exploring what a “good death” could look like and what my father would want.
Read the rest of this entry »
New Year is a good time for Veterans to review benefits
The New Year is a time for resolutions and fresh starts. For veterans it’s also a good time to review their benefits with a professional to ensure they are receiving the benefits they have earned through their service and sacrifice.
“All veterans should occasionally check with a Veterans Service Officer to see if changes in a veteran’s circumstances or changes to benefit policies may have modified the programs a veteran may be eligible to receive,” said Brian Natali, chief, Division of Veterans Services and Programs with the Pennsylvania Department of Military and Veterans Affairs (DMVA). “Veterans should take these important steps to secure their benefits, and there are numerous accredited Veterans Service Officers and organizations eager to help.”

The easiest way to manage military documents is to make sure they are filed in a safe place immediately upon leaving the military. Veterans often find that filing their documents for free at their county courthouse of record is an easy way to secure them until needed, which can often be decades into the future.
Another key step, says Natali, is for veterans to apply for federal health care and state benefits by visiting their local county director of veterans affairs or area accredited service organizations to take a look at what benefits they may be eligible for and to get help applying for those benefits.
How to Plan, Prepare, and Realistically Pay for Long-Term Care
Published in caringfromafar.com
When you plan for your future, do you include any plans for long-term care? It’s an aspect of life that too many adults fail to properly plan for, and that can leave seniors and family members struggling to find a solution. So, if you really want to prepare beforehand, you need to make some smart plans to cope with and pay for long-term care.
Focus on Your Long-Term Care Strategy First
Use Medicare to Your Advantage
Before you begin setting aside funds for long-term care, it’s important to have a good idea of what that situation may look like for you or a loved one. For many older adults, this means taking a look at how Medicare will offset any long-term care needs. While Medicare and Medicaid offer little long-term care assistance, the former can offer peace of mind through Medicare Advantage plans. These supplemental plans cover more of your future care, but it’s important to know the enrollment dates so you don’t miss out on this opportunity.
Know What Factors Put You at Risk
Another smart way to plan for long-term care is to examine your family history and lifestyle choices. For example, seniors with Alzheimer’s are likely to need progressive long-term care, and this is a condition which tends to be passed on from one generation to the next. But knowing you have a risk of developing dementia or Alzheimer’s also allows you to make changes in your life to potentially halt the impact of these illnesses. You can exercise more, change your diet, and even use puzzles and games to help decrease your need for long-term care in the near future. Cognitive decline is a major risk factor for long-term care, but serious falls can be a culprit as well. Also, dedicate some time to making your home a safe spot to age in place.
Put Together Your Plan to Pay for Care
Assess Your Insurance Coverage Options
You know that Medicare Advantage plans can help seniors stay better prepared for the future, but do you know how Medicare or health insurance covers long-term care costs? This may be a shock, but Medicare and Medicaid offer minimal long-term care coverage. In fact, the only aspects most health insurance plans will pay for are actions directly related to your health. So, the more routine care that most long-term care seniors need likely won’t be included in your average healthcare coverage. For many seniors, this is where options like long-term care insurance come in handy. If you plan ahead, this supplemental coverage is not as expensive and can offset some of the financial burdens. Understanding this kind of coverage can be a challenge, so make sure you carefully read through and research policies before you commit.
Research Other Viable Ways to Pay for Care
Medicare may not help, and long-term care insurance is not the perfect option for everyone. So, how can seniors find other ways to make sure they get the long-term help needed? Thankfully, there are some smart solutions to help give seniors and their families financial peace of mind. If you have served in the military, you may be eligible for more comprehensive VA coverage for your future care needs. It’s a benefit many veterans and loved ones forget, but this assistance is priceless for those struggling to find ways to afford long-term care. For adults who are not veterans, there may still be tools to help with costs. Financial assistance is available for seniors and family caregivers, but you can also reduce the expenses of care by carefully researching facilities and care providers. In essence, you can cut down your expenses by planning ahead.
Long-term care doesn’t have to be stressful, expensive, or, most importantly, an afterthought. It’s an essential step most adults will likely face at some point in the future. So, you should plan for long-term care just like you do any other important aspect of life and give yourself and your family some needed peace of mind in the process.
How to Help Your Loved One Stay in Touch with You

During the holidays, relatives will especially rely heavily on two-way communication to stay connected.
Published in caringfromafar.com
Technology makes communicating with your loved one as easy as the push of a button, which is a true blessing for long-distance caregivers. However, your loved one might not be as tech-savvy as you are, or they may have trouble communicating due to vision or hearing deficiencies. The following are simple ways to make staying in touch a breeze:
Start with the Basics
You might have gotten rid of your landline phone years ago, but for older adults, this is the phone they grew up using and are most comfortable with. Technology is confusing, and trying to teach your loved one how to use it could be more stressful than it is helpful. In fact, a landline phone may even be the safest option, as it reduces time spent routing the call to the correct emergency response center. In addition, calls from landlines automatically show emergency responders the address, name of the residence, and a map, which could be a lifesaver should your loved one call for help and be unable to talk or get confused about where they are.
Depending on your loved one’s needs, you can switch out the landline for something more feasible such as a phone with larger buttons or a high ringer volume. Keep in mind that getting your loved one a cell phone, and teaching them how is use it, is still a good idea, as they can take it with them when they are out of the house. To really ramp up the communication measures, install a medical alert system that makes communication with emergency services quick and simple.
Set a Schedule
Once you choose the preferred communication, set up a time each day to check in and stick to it. This not only gives you peace of mind that your loved one is okay, but even simply hearing a familiar voice could be the daily pick-me-up they need. If your loved one is tech-savvy, use video chat such as Skype or FaceTime, or have a local family member or in-home caregiver assist them.
In addition to communication with your loved one, it is imperative that you chat regularly with their primary caregiver to get details and information your loved one might not feel comfortable sharing with you. If you chose to hire an in-home caregiver, check in with them daily, and don’t be afraid to request a log of what they did each day. Don’t forget to ask your loved one how they feel – sometimes caregivers aren’t the right match.
Staying in touch with your loved one will take a continued effort on your end, but it is just one of the many responsibilities that come along with being a long-distance caregiver. With the right technology and a consistent schedule, you can make the miles between you seem far less.